Connect With Us
Featured Articles

Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.
The Wagner Diabetic Foot Ulcer Classification System
If you suffer from diabetes, you may be familiar with the increased risk of developing poorly healing wounds on your feet. Small cuts, sores, or scrapes can go unnoticed due to neuropathy or nerve damage, and heal slowly because of poor circulation. These issues can make wounds grow larger and become infected, turning into diabetic foot ulcers (DFUs). There are various classification systems for describing the general characteristics of these wounds. Doctors who use the Wagner system classify DFUs by their severity, in a graded system ranging from 0 to 5. A Grade 0 ulcer means that the skin is intact. Grade 1 signifies a superficial ulcer on the outer layers of skin. Grade 2 is a deep ulcer. Grade 3 is an ulcer with bone involvement. Grade 4 means that there is gangrene or dead tissue in the front of the foot, while Grade 5 means that the gangrene has spread to the entire foot. If you notice any wounds on your feet, please schedule an appointment with a podiatrist who can treat wounds and help you manage your condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Rouder from S.I. Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
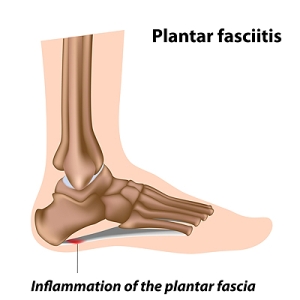
Am I at Risk for Plantar Fasciitis?
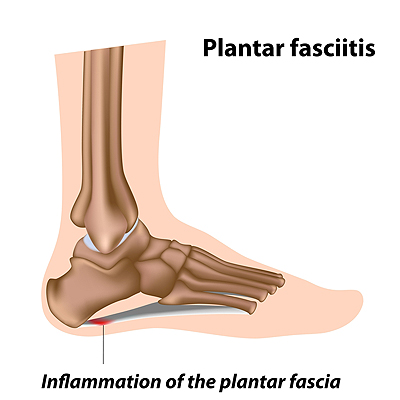 Plantar fasciitis is a very common foot problem, especially among runners. It occurs when the plantar fascia, the ligament that runs along the bottom of the foot and connects the heel bone to the toes, becomes inflamed due to repeated injury or overuse. You may be at an increased risk for developing plantar fasciitis if you are a highly active runner, stand for prolonged periods of times, have tight calves or a decreased range of motion in your ankles, have flat or high arched feet, or are obese. Fortunately, there are many treatments for plantar fasciitis, including resting the foot, performing foot stretches, and modifying your activities or footwear. If you believe that you are at risk for developing plantar fasciitis, please consult with a podiatrist.
Plantar fasciitis is a very common foot problem, especially among runners. It occurs when the plantar fascia, the ligament that runs along the bottom of the foot and connects the heel bone to the toes, becomes inflamed due to repeated injury or overuse. You may be at an increased risk for developing plantar fasciitis if you are a highly active runner, stand for prolonged periods of times, have tight calves or a decreased range of motion in your ankles, have flat or high arched feet, or are obese. Fortunately, there are many treatments for plantar fasciitis, including resting the foot, performing foot stretches, and modifying your activities or footwear. If you believe that you are at risk for developing plantar fasciitis, please consult with a podiatrist.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Rouder from S.I. Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
What to Do if You Stand All Day at Work
 If you have a job that requires you to stand all day, there are things you can do to alleviate swelling and pain to help prevent further foot complications from developing over time. Wear good shoes that offer support, cushioning, and stability—and when they get worn out, replace them. Custom orthotics designed and fit your individual foot by a podiatrist can help your feet withstand the pressure of standing all day. Compression stockings can help circulation and reduce swelling. When you get home from work, soak your feet in a warm bath, or try icing them to reduce swelling and massaging them to relieve sore muscles. You can also ask a podiatrist to suggest exercises that massage the heel, and stretch your feet, Achilles tendon, and calf muscles. A podiatrist may also be able to recommend the best type of shoe for your particular feet.
If you have a job that requires you to stand all day, there are things you can do to alleviate swelling and pain to help prevent further foot complications from developing over time. Wear good shoes that offer support, cushioning, and stability—and when they get worn out, replace them. Custom orthotics designed and fit your individual foot by a podiatrist can help your feet withstand the pressure of standing all day. Compression stockings can help circulation and reduce swelling. When you get home from work, soak your feet in a warm bath, or try icing them to reduce swelling and massaging them to relieve sore muscles. You can also ask a podiatrist to suggest exercises that massage the heel, and stretch your feet, Achilles tendon, and calf muscles. A podiatrist may also be able to recommend the best type of shoe for your particular feet.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact Dr. Rouder from S.I. Podiatry. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Working on Your Feet
Foot care is important regardless of your profession, but those who work on their feet must pay special attention. Bunions, calluses, blisters, and plantar warts are just a few of the many conditions that can arise after standing all day. While painful at their worst, these conditions can easily be avoided with the right foot care. This includes both appropriate footwear and proper posture—important elements that affect the health of your feet.
Choosing appropriate footwear means choosing a shoe that has a negative heel. This means that the heel is slightly lower than the ball of your foot, which places less of a strain. If you have a profession that requires you to be on your feet all day, investing in a pair of high-quality shoes is pertinent. High-quality shoes can be purchased from a respected manufacturer that emphasizes foot care and foot health.
Despite the regularity of wearing shoes, the feet are naturally not designed to be enclosed. Regular “barefoot” time for your feet can be beneficial for foot health. Among other methods, allowing your feet to breathe can help alleviate the pain and pressure your feet may be experiencing from being on your feet all day.
Simple foot exercises and yoga positions can help improve both the health and function of your feet. Active foot exercises that create movement will stimulate your foot’s blood flow and circulation, and yoga positions that place your feet flat onto the floor will stretch out their muscles. Yoga is particularly beneficial for your Achilles tendon and calf muscles, which are areas that can become especially problematic if not taken care of. Foot exercises and yoga positions can be easily performed every day at virtually any location and any time; whether it is at the office, at the gym, or at home right before you go to bed. Simple stretching can increase your foot health by miles.
The foot pain you experience after lengthy hours working on your feet may seem inevitable and unavoidable; in reality, however, that is not the case. Wearing proper footwear and performing simple foot exercises and stretches can help ease foot pain and allow you to truly avoid frustrating foot problems.
Your feet can easily be kept healthy with some education and a little effort. Pain that begins at the feet can eventually affect the whole body. Begin taking care of your feet now!
Can Salicylic Acid Treat Plantar Warts?
Salicylic acid is a topical solution that can help the skin shed dead cells from its top layer and can reduce inflammation and redness of the skin. Salicylic acid is sometimes prescribed as a treatment for plantar warts. Plantar warts are the hard, grainy bumps that grow on the bottom of the feet as a result of a human papillomavirus (HPV) infection. While there are salicylic acid treatments that can be bought over the counter, the thicker skin on the soles of the feet may require a prescription strength solution. If you have plantar warts, it is suggested that you consult with a podiatrist to find the right treatment for you.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Rouder from S.I. Podiatry. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Causes of Cracked Heels
A condition referred to as cracked heels is often uncomfortable and may produce severe pain. It is a common foot ailment that many people experience. Cracked heels occur when the skin on the back of the heel becomes dry, possibly be due to a lack of moisture in the skin or the amount of pressure the heels endure on a daily basis. This condition may be a result of poor dietary lifestyle habits, standing on your feet for most of the day, or wearing improper footwear. Relief options may be obtained by soaking the feet in warm water, followed by utilizing an adequate foot cream that can help to soften the skin. Additionally, it may be beneficial to file down the skin surrounding the cracks, which are often referred to as fissures. It is strongly suggested to seek the advice of a podiatrist for additional information and proper treatment options for cracked heels.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Dr. Rouder from S.I. Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.